Iliotibial Band Friction Syndrome – Explained
August 17, 2018 / Nev Davies FRCS (Tr. & Orth.) Consultant Orthopaedic Surgeon
This blog explains the relevant anatomy, clinical features and treatment strategies for Iliotibial band friction syndrome, which is a common cause of pain on the outside of the knee, caused by inflammation as the tendon rubs over the bone.
It’s a very common cause of lateral (outside) knee pain in runners.
What is the iliotibial band (ITB)?
The ililotibial band (ITB) is a tube shaped tendinous structure that is formed from the confluence of the lateral covering structures of the outer muscles of the buttocks and thigh. It passes down the outer side of the leg, crossing the knee and inserting into a bony prominence on the front of the tibia (shin bone) known as Gerdy’s tubercle. (See Picture 1 below)
A1 – Gluteus Maximus (buttock muscle)
A2 – Tensor Fascia Lata muscle (TFL) – thigh muscle
B – Fascia Lata (covering of muscles)
C – Iliotibial band (ITB) – tube shaped confluence of fascia lata
D – Gerdy’s tubercle – bony lump
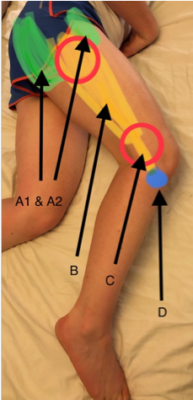
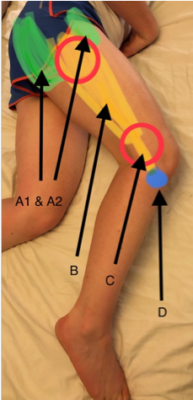
Picture 1 – clinical photograph of the outer aspect of thigh
How does ITB friction syndrome present?
It usually comes on gradually over time as an athlete may increase their amount of training. (overuse injury) It can get progressively worse until eventually running becomes really difficult. Typically it’s aggravated by running downhill and as it gets steadily worse the patient will have to rest for a time until symptoms settle, only for them to return when training resumes.
How is it diagnosed?
Usually ITB friction syndrome is a clinical diagnosis so is made by taking a good history and performing a sound clinical examination. Most patients will be sore around the lateral, outer aspect of the knee as the ITB passes down across the joint and inserts into Gerdy’s tubercle. Often patients will have tight lateral structures which can be assessed using Ober’s clinical test. (see Video 1)
Video 1 – Ober’s test
It is important to examine the biomechanics of the lower legs as often foot position, muscle imbalance around the gluteal muscles and running technique can play a role in who is susceptible to this condition.
Do I need an MRI scan?
Although ITB friction syndrome can be diagnosed clinically, an MRI scan (see picture 2) is useful to confirm the diagnosis, rule out other pathology in the knee and also look at an individual’s specific anatomy. As MRI scans become more accurate in showing all the tissues in great detail, they are becoming the imaging of choice for the knee specialist.
Picture 2 – MRI scanner
Non-operative treatments are always suggested and should be tried first and these should be guided by a good sports physiotherapist. The root cause of the overload of the ITB needs to identified and then addressed.
Physiolistic are a specialist sports physiotherapy clinic based in Henley-on-Thames – led by director Angela Botha and her team have a wealth of knowledge and all the latest techniques for treating ITB syndrome.
Stretching out tight lateral structures with specific exercises and also using a foam roller (see Video 2) regularly is a really good starting point. Addressing muscle control and weakness of the hip, knee and ankle also need to be implemented.
Video 2 – using a foam roller to loosen tight lateral structures
Icing the knee after activities will combat acute inflammation and often the pain is helped by an anti-inflammatory medicine such as ibuprofen. It’s important to take these with food as they can cause stomach upsets.
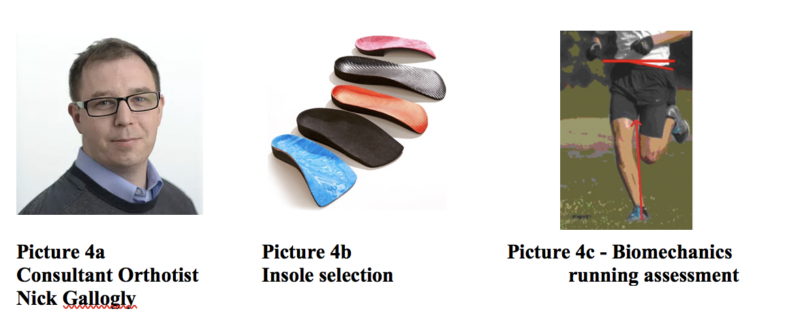
Sometimes as well as physiotherapy I will refer patients to my specialist orthotist colleague Nick Gallogly – Nick may prescribe some orthotics (insoles) to alter the foot position which in turn influences the mechanics across the knee. He also carries out gait assessment and offers advice on footwear for running.
Recalcitrant problems are dealt with a more aggressive approach, usually starting with an ultrasound guided injection of steroid medicine into the inflamed area as one option.
Failing all these measures – day case surgery under a general anaesthetic to debride and lengthen the tendon, and hence encourage a healing response, is a last resort but usually has a good outcome.
If you think you have ITB syndrome or any other knee issues and would like to see me in clinic to discuss further please contact my Private Secretary Debbie Rollason on 07305 097 137 or via email: nevdavies.secretary@gmail.com
Physiolistic – Specialist Sports injuries and Physiotherapy Clinic
Based in the Henley Rugby Club grounds. We aim to get to the root cause of your ITB problem and then have individually tailor your treatment and rehabilitation
Purpose built clinic with free parking outside. Open 7 days a week. Book online at www.physiolistic.co.uk or call 01491 598043 or email info@physiolistic.co.uk
Nick Gallogly (Consultant Orthotist) sees patients at Circle Reading, Spire Dunedin and Physiolistic. – for an appointment please call his secretary Jane Hardie on 07885651450 or email: secretary.orthotics@gmail.com
Nev is a local expert knee surgeon with his NHS practice at the Royal Berkshire Hospital and private practice consulting at both Spire Dunedin and Circle Reading Hospital. He treats adult knee problems but also has subspecialist interest in childrens’ and adolescents’ orthopaedic conditions. He is a member of Reading Hip and Knee Unit, Reading Foot and Ankle Unit and Reading Children’s Orthopaedic Unit. He is passionate about education and teaching – if you are a healthcare provider and would like to come and sit in on clinic, or come to the operating theatre to observe surgery this can be arranged. Also, if you would like Nev to visit your practice and give a talk about anything trauma or orthopaedic related then please get in touch.



